Plasma fibroblast therapy has gained attention in aesthetic medicine as a non-surgical option for addressing certain skin concerns. However, like many aesthetic treatments, its effectiveness and safety depend largely on whether the individual is an appropriate candidate. Not everyone will benefit equally, and responsible providers emphasize careful assessment over universal suitability.
At FibroblastUSA, we focus on education-first guidance around plasma fibroblast technology, including the Plamere device, so practitioners and patients alike understand who may be appropriate for this treatment—and who may not. In this article, we explore the characteristics of ideal candidates for plasma fibroblast therapy, grounded in current dermatologic understanding and professional best practices.
Important note: Plasma fibroblast therapy is not a medical cure or guaranteed solution. Individual outcomes vary, and all treatments should be performed by trained professionals following proper evaluation.
What Is Plasma Fibroblast Therapy?
Plasma fibroblast therapy is a non-surgical aesthetic procedure that uses a controlled plasma arc to create micro-injuries on the surface of the skin without direct contact. This plasma arc is generated by ionizing gases in the air between the device tip and the skin’s surface. The thermal effect is localized and superficial, primarily affecting the epidermal layer.
The treatment is based on the biological role of fibroblasts, which are cells involved in collagen and elastin production. When the skin undergoes controlled trauma, fibroblast activity may increase as part of the natural wound-healing response. Over time, this process may contribute to changes in skin texture and firmness.
The Plamere plasma fibroblast device is designed to deliver consistent plasma output when used according to training protocols. As with all aesthetic devices, results depend on practitioner skill, patient characteristics, and adherence to safety guidelines—not on the device alone.
Plasma fibroblast therapy differs from surgical procedures in that it does not involve incisions, sutures, or general anesthesia. However, it is still a procedure that affects the skin and must be approached with clinical responsibility.
Why Candidate Selection Matters
Candidate selection is one of the most critical aspects of plasma fibroblast therapy. Inappropriate treatment can increase the risk of adverse effects such as prolonged healing, pigmentation changes, or unsatisfactory outcomes.
Factors such as skin type, degree of skin laxity, medical history, and healing capacity all influence whether plasma fibroblast therapy is appropriate. Ethical providers prioritize patient safety and realistic expectations rather than offering one-size-fits-all solutions.
From a clinical perspective, plasma fibroblast therapy is best viewed as a selective aesthetic option, not a replacement for surgical intervention or comprehensive dermatologic care.
General Characteristics of Ideal Candidates
Mild to Moderate Skin Laxity
Plasma fibroblast therapy is generally considered most suitable for individuals with mild to moderate skin laxity. This may include early signs of aging such as fine lines, crepey skin, or slight loss of firmness. It is not designed to correct significant skin sagging or structural changes.
Adults With Stable Skin Health
Candidates are typically adults over the age of 18 with generally healthy skin. While many individuals seeking treatment fall between their 30s and 60s, chronological age alone does not determine suitability. Skin condition and healing ability are more relevant than age itself.
Realistic Expectations
An ideal candidate understands that plasma fibroblast therapy does not produce immediate or dramatic transformations. Changes occur gradually as part of the skin’s natural healing response. Multiple sessions or maintenance treatments may be considered, depending on individual goals and professional recommendations.
Skin Types and Plasma Fibroblast Therapy
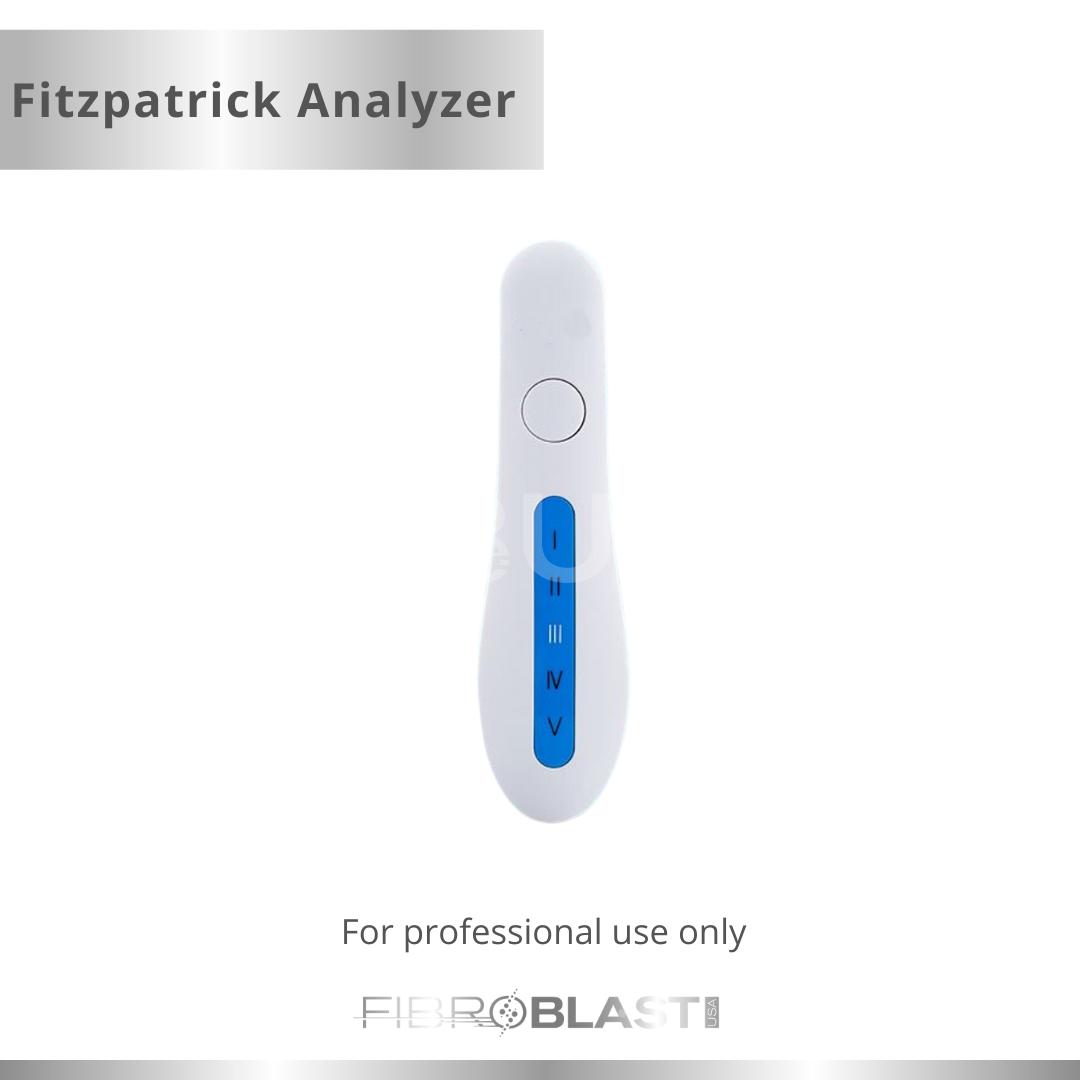
Fitzpatrick Skin Type Considerations
Skin type plays a significant role in plasma fibroblast therapy planning. Individuals with Fitzpatrick skin types I–III are often considered lower risk for pigmentation-related side effects. Those with Fitzpatrick types IV–VI may have a higher risk of post-inflammatory hyperpigmentation (PIH).
This does not automatically exclude darker skin tones, but it does require heightened caution, advanced practitioner experience, and strict pre- and post-treatment protocols.
Pigmentation Risk Awareness
Because plasma fibroblast therapy involves thermal skin interaction, pigmentation changes are a known consideration. Proper patient screening, conservative energy settings, and diligent aftercare are essential to minimizing risk.
A professional consultation is necessary to evaluate whether the potential benefits outweigh the risks for each individual.
Common Treatment Areas and Candidate Suitability
Plasma fibroblast therapy is typically used for localized skin concerns, not large treatment zones.
Eyelids (Upper and Lower)
Mild eyelid laxity is one of the most commonly discussed applications. Suitable candidates have early skin looseness without significant fat prolapse or structural drooping that would require surgical correction.
Perioral Area
Fine lines around the mouth may be addressed in select cases. Plasma fibroblast therapy does not add volume and is not a substitute for dermal fillers.
Neck and Décolletage
Early texture changes in the neck and chest area may respond differently than facial skin due to thinner dermal layers. Conservative treatment planning is essential.
Body Areas
Small areas such as knees, arms, or abdomen with mild laxity may be considered on a case-by-case basis.
Who May Not Be an Ideal Candidate
Plasma fibroblast therapy is not appropriate for everyone. Individuals may be advised against treatment if they have:
- Active skin infections or inflammatory skin conditions
- A history of poor wound healing or keloid scarring
- Certain autoimmune or connective tissue disorders
- Recent isotretinoin (Accutane) use
- Pregnancy or breastfeeding (as a precautionary measure)
Additionally, individuals seeking guaranteed or immediate results may not be suitable candidates. Ethical aesthetic practice prioritizes patient safety over treatment eligibility.
Pre-Treatment Evaluation and Professional Consultation
A comprehensive consultation is essential before any plasma fibroblast procedure. This includes:
- Review of medical and dermatologic history
- Assessment of skin type and condition
- Discussion of risks, limitations, and aftercare
- Informed consent
At FibroblastUSA, we emphasize that Plamere devices are tools, and their safe use depends on practitioner training, experience, and adherence to protocols.
Safety, Regulation, and Evidence-Based Practice
Plasma fibroblast therapy exists within the broader field of aesthetic medicine, which continues to evolve through clinical experience and research. While components of plasma technology are used in various medical applications, aesthetic plasma fibroblast procedures should always align with state regulations and scope-of-practice laws.
Practitioners should rely on peer-reviewed dermatologic principles, manufacturer training, and conservative treatment planning rather than exaggerated claims. Responsible education and transparent communication remain central to patient trust.
Key Takeaways: Is Plasma Fibroblast Therapy Right for You?
Plasma fibroblast therapy may be an option for select individuals seeking non-surgical skin treatments, particularly those with mild to moderate skin laxity and realistic expectations. However, it is not universally appropriate and should never be positioned as a guaranteed solution.
The Plamere plasma fibroblast device is one component of a broader treatment approach that prioritizes patient evaluation, safety, and ethical practice. A qualified consultation is the most important step in determining suitability.
At FibroblastUSA, we believe informed decisions lead to better outcomes—for both practitioners and patients.
Frequently Asked Questions (FAQ)
What is plasma fibroblast therapy used for?
Plasma fibroblast therapy is used in aesthetic practice to address certain mild to moderate skin concerns, such as fine lines, skin texture irregularities, and early skin laxity. It works by creating a controlled plasma arc on the skin’s surface, which initiates a natural healing response. It is not intended to replace surgical procedures or treat medical skin conditions.
Who is considered an ideal candidate for plasma fibroblast therapy?
Ideal candidates are typically adults with mild to moderate skin laxity, generally healthy skin, and realistic expectations. Suitability depends on factors such as skin type, medical history, and healing ability. A professional consultation is essential to determine whether plasma fibroblast therapy is appropriate for an individual.
Is plasma fibroblast therapy suitable for all skin types?
Plasma fibroblast therapy is not universally suitable for all skin types. Individuals with lighter skin tones (Fitzpatrick I–III) may have a lower risk of pigmentation-related side effects. Those with darker skin tones (Fitzpatrick IV–VI) may still be considered but often require additional caution, conservative settings, and experienced providers due to increased pigmentation risk.
How does the Plamere plasma fibroblast device work?
The Plamere device generates a controlled plasma arc by ionizing gases in the air between the device tip and the skin. This creates superficial thermal micro-injuries without direct contact. The device itself does not determine results; outcomes depend on practitioner training, treatment planning, and individual skin response.
Is plasma fibroblast therapy a non-surgical alternative to cosmetic surgery?
Plasma fibroblast therapy is considered non-surgical, as it does not involve incisions or sutures. However, it is not equivalent to surgical procedures and is not appropriate for significant skin laxity or structural concerns. Patients seeking dramatic or immediate changes may require surgical consultation instead.
How long does it take to see changes after plasma fibroblast therapy?
Skin changes typically develop gradually over several weeks as part of the body’s natural healing process. Individual timelines vary based on skin condition, age, aftercare, and biological response. Immediate results should not be expected.